Επιλεγμένες Επιστημονικές Δημοσιεύσεις
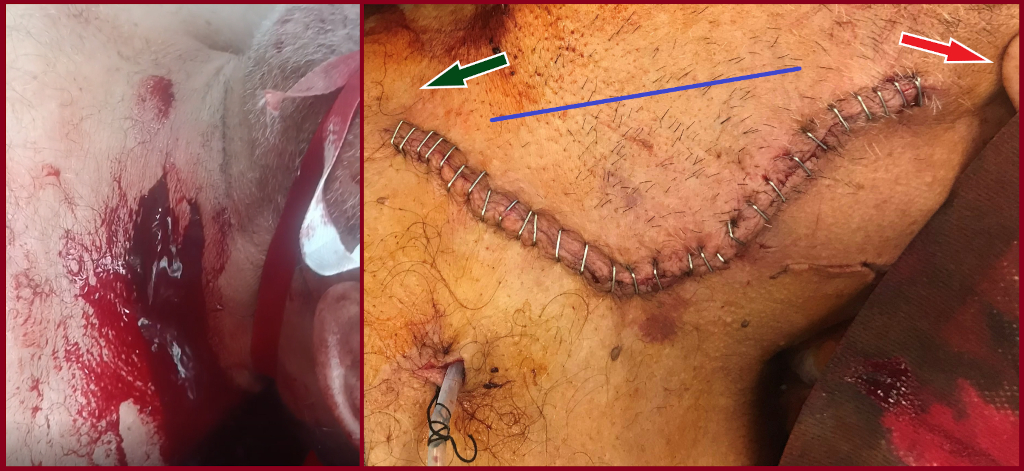
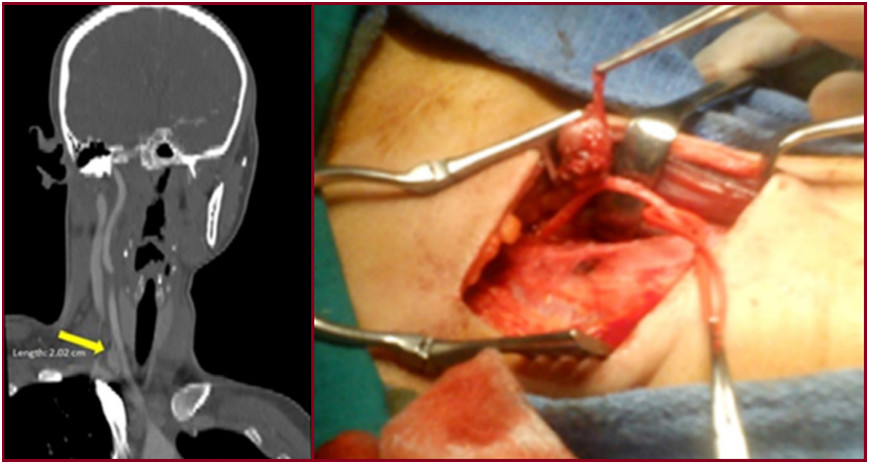
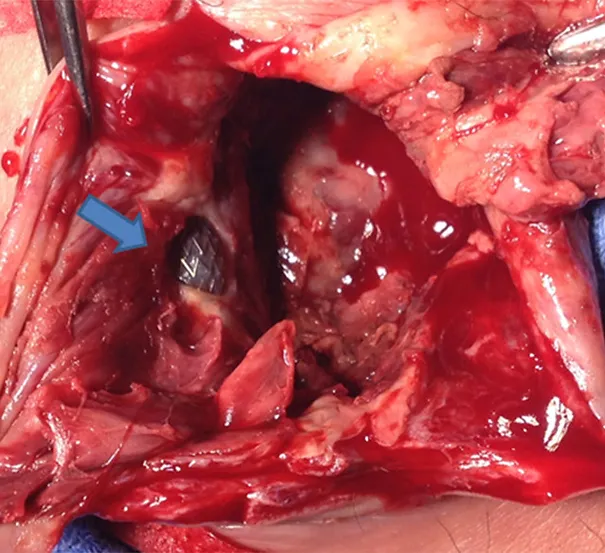
Penetrating internal jugular vein injury with massive bleeding
S. Papadoulas et al. Pol J Thoracic and Cardiovascular Surg 2025; 22 (2): 126-128. doi: https://doi.org/10.5114/kitp.2025.152193. Department of Vascular Surgery, University of Patras Medical School, Patras, Greece
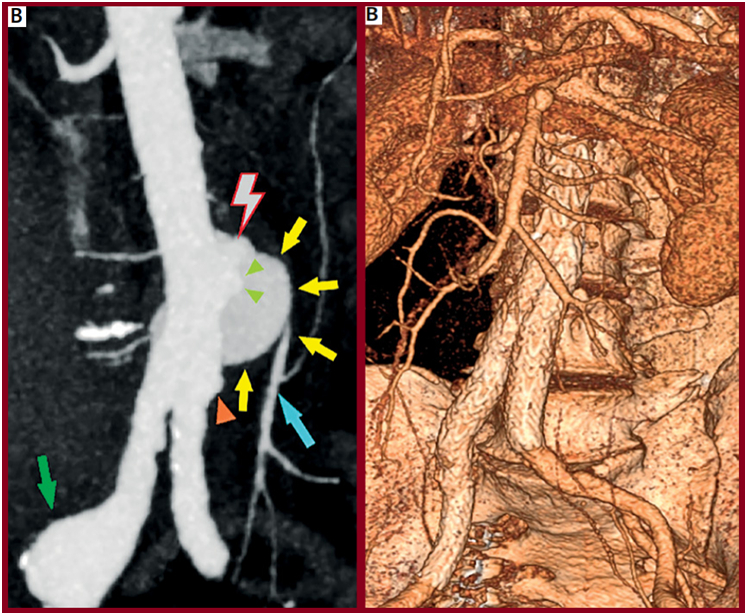
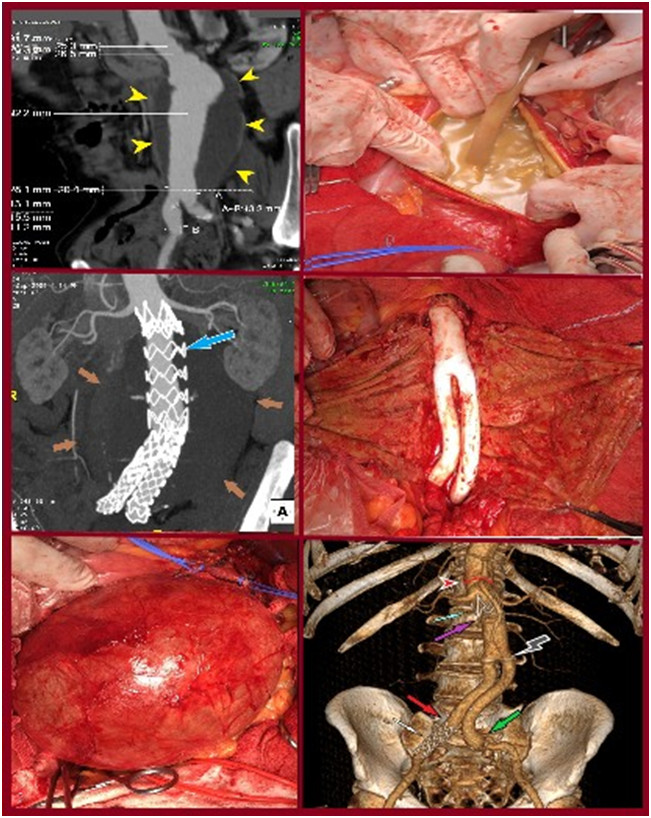
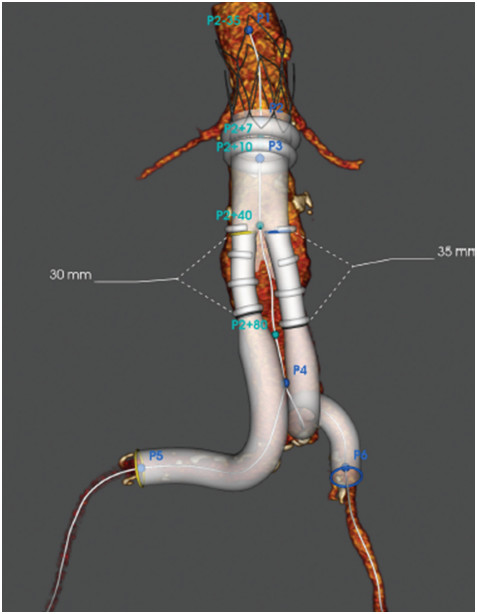
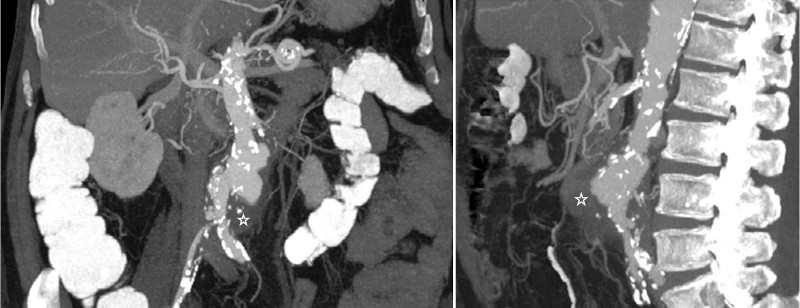
Spontaneous avulsion of the inferior mesenteric artery in a neurofibromatosis type 1 patient: a case-based review
S.Papadoulas et al Arch Med Sci Atheroscler Dis 2025; 10: e48–e68 doi:https://doi.org/10.5114/amsad/205022. Department of Vascular Surgery, University of Patras Medical School, Patras, Greece
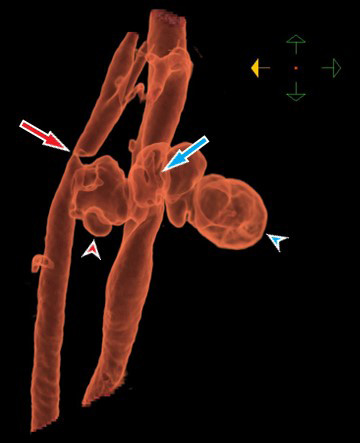
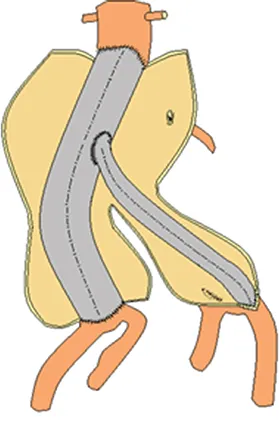
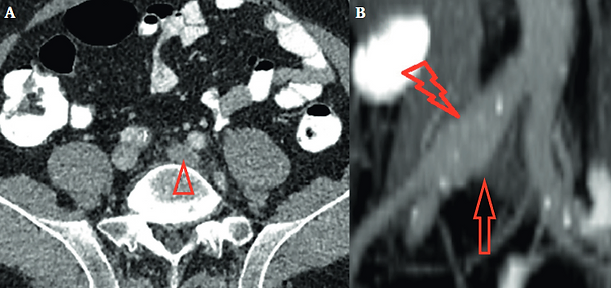
We present the case of successful endovascular abdominal aortic aneurysm repair (EVAR) in a 55-year-old male who presented with a ruptured infrarenal aortic pseudoaneurysm, formed after spontaneous avulsion of the inferior mesenteric artery. The avulsion occurred after lifting a heavy object. Although aortic endografting is not the first option in patients with hereditary disorders due to aortic friability and concerns about long-term durability, it is valuable in urgent cases due to lower morbidity and mortality, even as a bridging procedure. This policy is further supported by the fact that the alternative open reconstruction has been invariably associated with hemostasis issues and poor outcomes due to arterial fragility and inability to construct safe anastomoses. Finally, we present a current literature review regarding abdominal aortic and iliac pathology in patients with neurofibromatosis type 1 focusing on the type of the vascular lesion, method of repair and outcome.
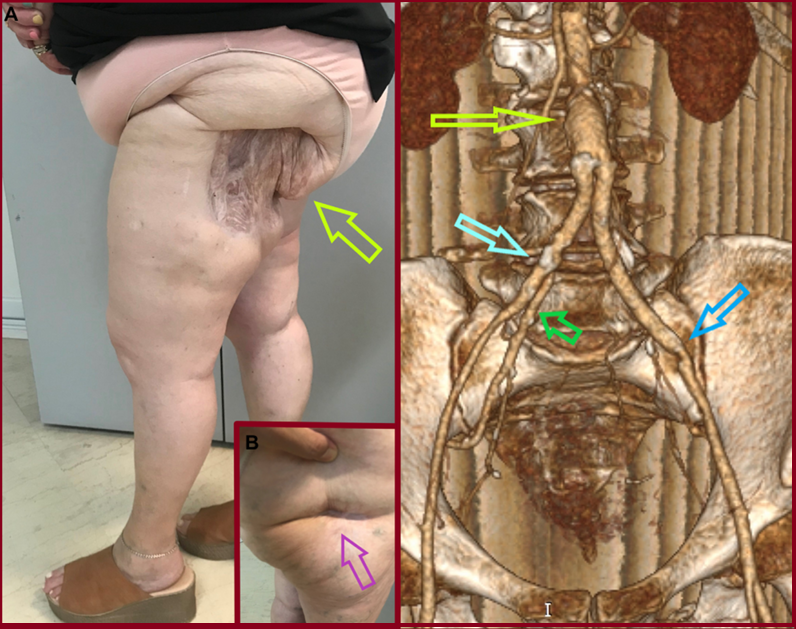
Gluteal ischemic gangrene due to chronic aortoiliac occlusive disease
C. Pitros, S. Papadoulas et al. J Vasc Surg Cases Innov Tech 2025;11:101792. Department of Vascular Surgery, University of Patras Medical School, Patras, Greece
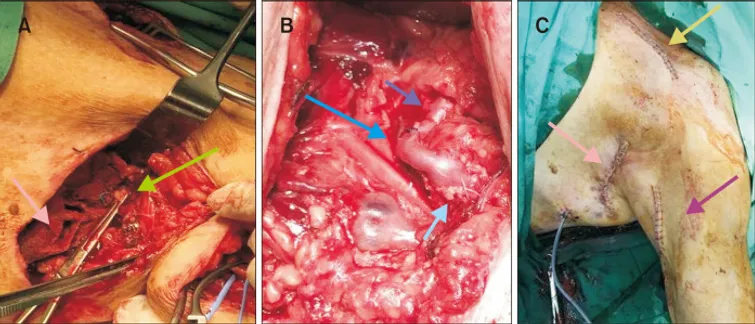
Gluteal gangrene rarely complicates interventional procedures such as angiographic embolization in the pelvis or may develop postoperatively after open ligation or endovascular covering or embolization of one or mainly both internal iliac arteries in abdominal aortic surgery if collateral circulation is compromised. On the other hand, gluteal gangrene as a primary manifestation of chronic aortoiliac occlusive disease is very exceptional in literature. We present a patient with atherosclerotic aortoiliac obstruction and a necrotic eschar on her left buttock treated with aortobiiliac bypass after digital subtraction angiography. Internal iliac artery revascularization, even contralaterally, is crucial for the healing of necrotic tissue in these patients.
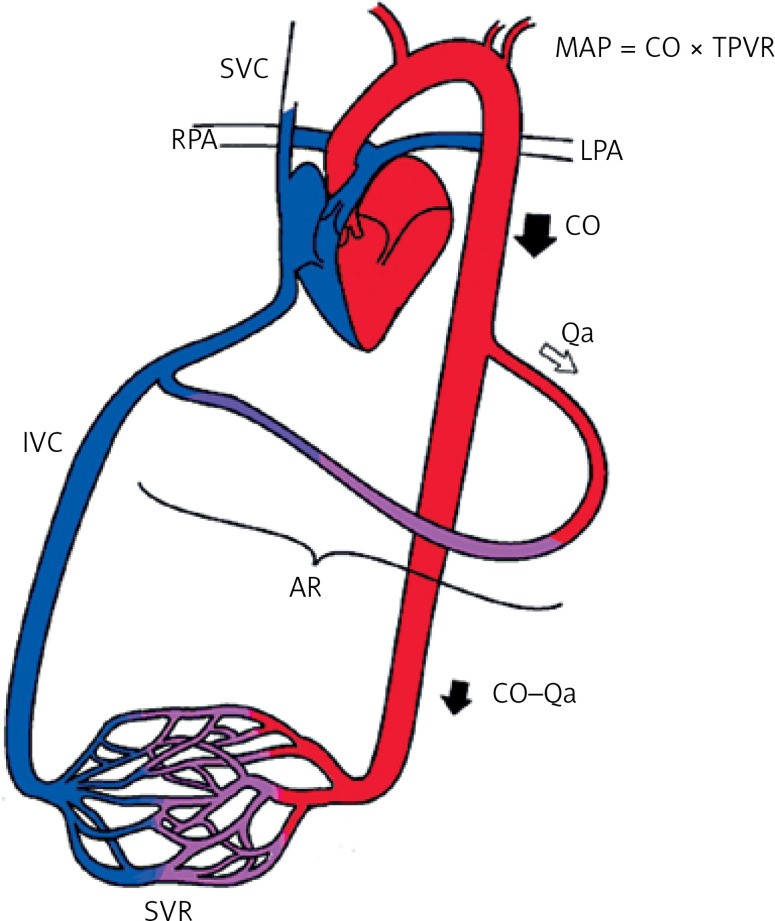
Cardiac complications of arteriovenous access: a narrative review from a multidisciplinary team perspective
Stathopoulou, S. Papadoulas et al. Arch Med Sci Atheroscler Dis 2024; 9: e217–e225. Department of Vascular Surgery, University of Patras Medical School, Patras, Greece
Although cardiovascular disease is common among hemodialysis patients, arteriovenous access creation has been invariably implicated in the evolution of adverse cardiac outcomes or deterioration of pre-existing cardiovascular disease. In most cases, these effects are subclinical but with potential underlying echocardiographic findings. Compared with grafts, arteriovenous fistulas are implicated more often, due to the progressively increased flow from the continuous dilatation of the venous outflow tract in the long term. The increasing flow is in the majority of patients well tolerated by cardiac adaptive alterations. However, the clinical impact is based on the balance between the amount of flow volume and the patient’s cardiac reserves. Having extensively reviewed the existing English literature, we present the pathophysiology and the different types of cardiovascular complications, the indications, types, and efficacy of flow-restrictive procedures in the con text of a high-flow AVF, as well as some precautions and considerations for AVF creation in high-risk patients.
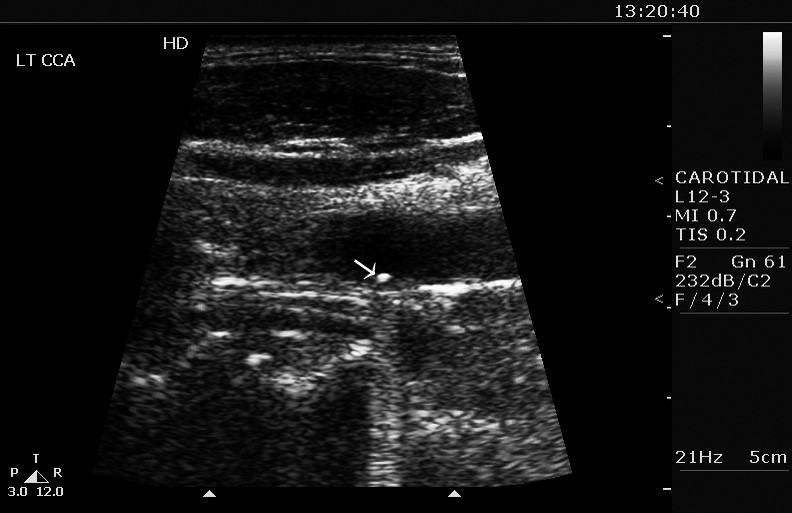
Penetrating carotid artery injury
V. Argitis, S. Papadoulas et al. Hellenic Journal of Vascular and Endovascular Surgery | Volume 6 – Issue 2 – 2024. Department of Vascular Surgery, University of Patras Medical School, Patras, Greece
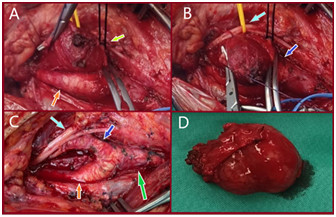
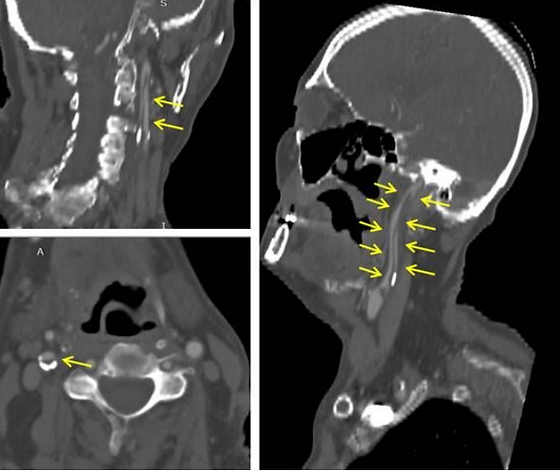
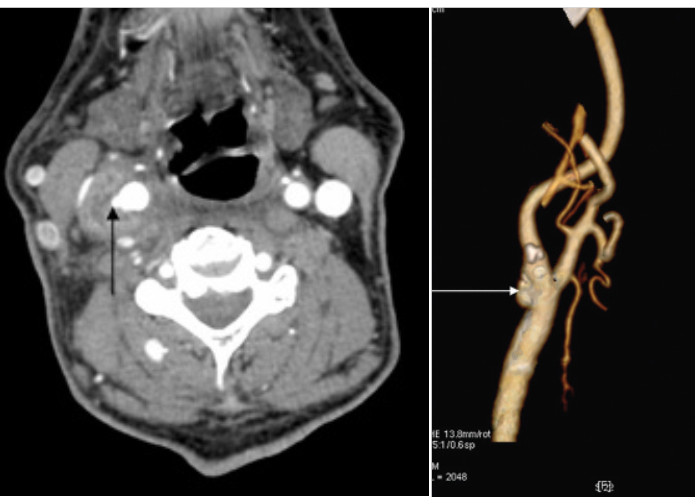
A 27-year-old male presented with a left cervical pulsative mass after penetrating trauma with a knife. No external bleeding was observed despite the presence of an open skin incision over the sternocleidomastoid muscle. Urgent Computed Tomography Angiography (CTA) revealed a partial transverse transection of the left common carotid artery (CCA) and the adjacent internal jugular vein (IJV) surrounded with a cervical hematoma due to gross extravasation from both vessels (Figure). In operating theatre, after a standard open approach for carotid endarterectomy, the CCA and IJV were clamped. The CCA was totally transected at the injury site, trimmed and re-anastomosed in an end-to-end fashion. The IJV was primarily sutured, and the hematoma was evacuated. The postoperative care was uneventful, and the patient was discharged on the 4th postoperative day. She was prescribed single antiplatelet and antibiotic treatment
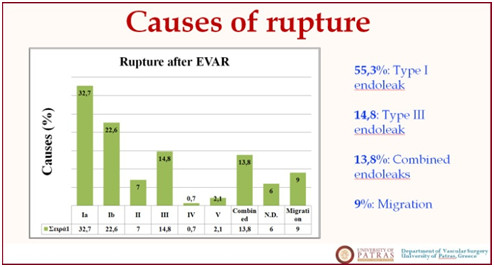
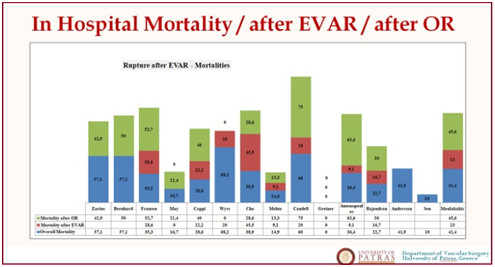
Late post-EVAR abdominal aortic aneurysm rupture: a meta-analysis study
The perivascular hypodense rim in carotid body tumor surgery
The ‘hook-sign’ in the Median Arcuate Ligament Syndrome
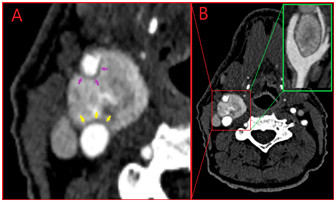
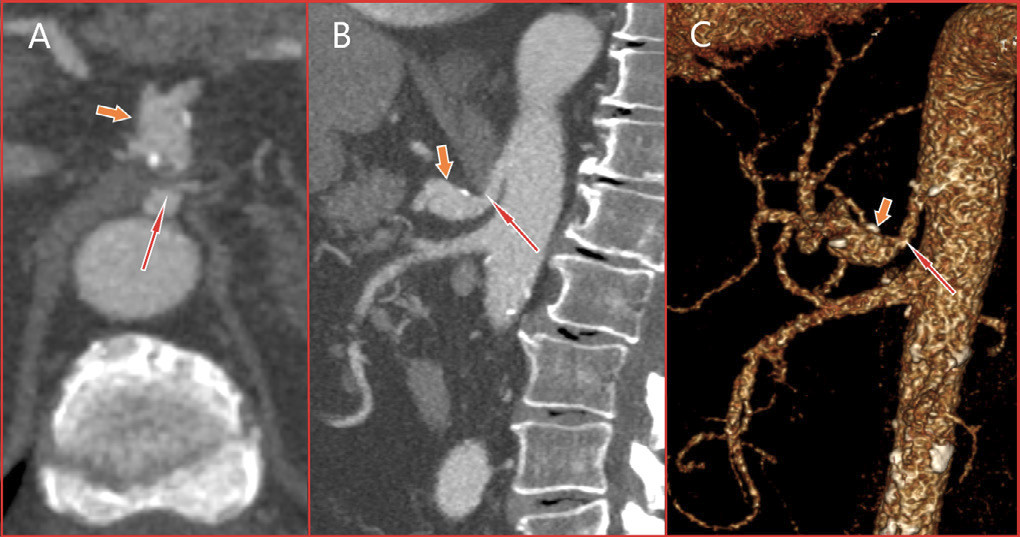
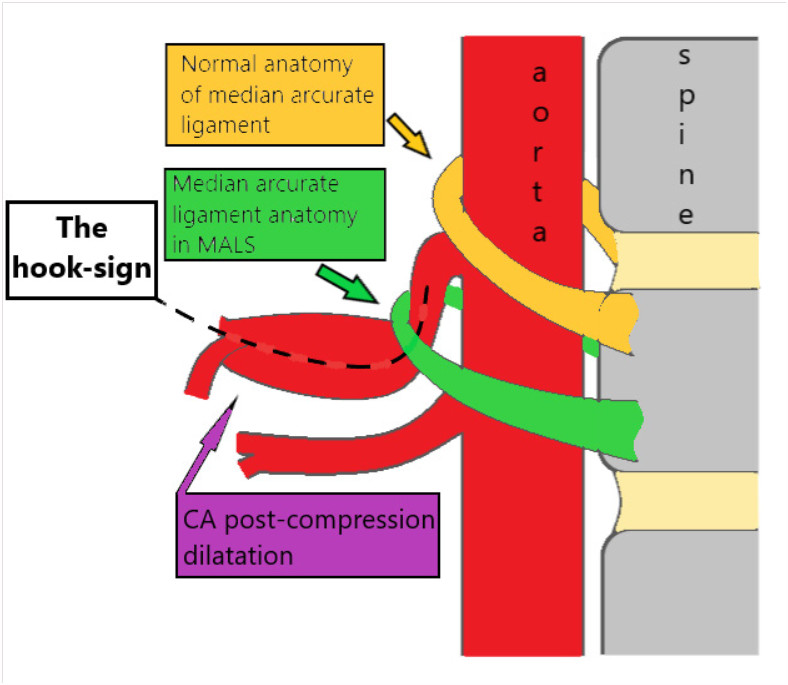
An 83-year-old male, former smoker with a medical history of hypertension and a thoracic aortic aneurysm was presented complaining of itching and edema of his legs. Symptoms were attributed to tactile skin purpura. An abdominal computed tomography (CT) scan was performed to rule out a para-neoplasmatic syndrome. An asymptomatic compression of the celiac artery by the median arcuate ligament (MAL) along with celiac artery kinking and a significant post-compression dilatation (15x15mm in size) was depicted. A following CT An-giogram (CTA) delineated the arterial anatomy and suggested the co-existence of an asymptomatic median arcuate ligament syndrome (MALS), (Figure 1). Median arcuate ligament syndrome was first described in 1917 by Lipshutz who noticed the overlapping of the artery by the diaphragmatic crura in an autopsy. It is a rare condition characterized by recurrent episodes of epigastric pain, nausea, diarrhea, and weight loss. The pain tends to be postprandial with a recession when leaning forward. Symptomatology is attributed to celiac artery compression by the arch-shaped ligament. Lower origin of the celiac artery or superior position of the MAL may predispose to MALS. The distortion of the CA centerline creates the ‘hook-sign’ (Figure 2). Sometimes, a neuropathic pain may be apparent due to ischemia or compression of the celiac ganglion. Current treatment consists of laparoscopic ligament transection followed by celiac artery angioplasty. A post-stenotic aneurysm larger than 2cm is generally
repaired by covered-stents or open surgery.
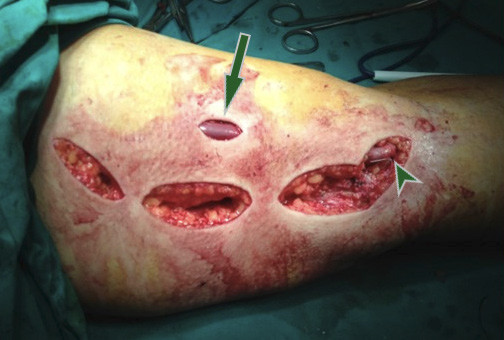
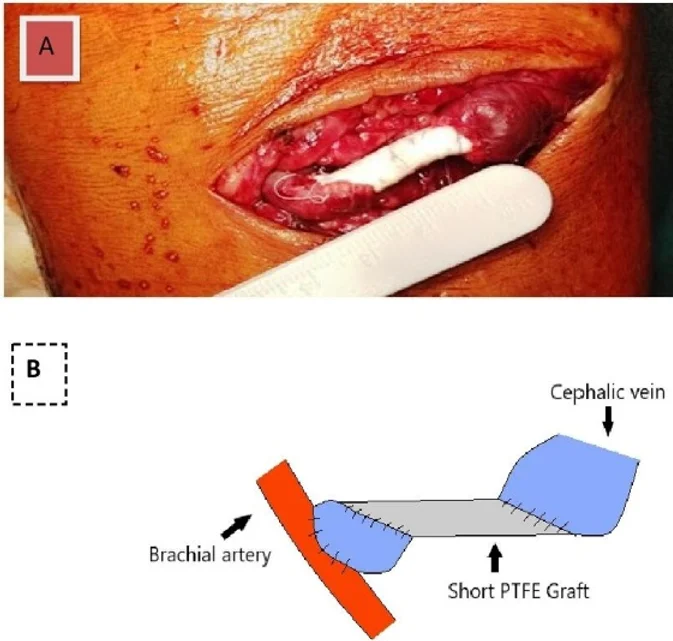
Multiple skip incisions technique for two-staged basilic vein transposition: a good alternative to the standard single long incision
A 58-year-old-male on hemodialysis underwent a two-staged tunneled basilic vein transposition with three skip incisions. Initially, preoperative color-duplex mapping was performed and a standard brachio-basilic arteriovenous fistula with the median cubital vein was accomplished. Six weeks later, after the arterialization of the basilic vein, the second stage took place after skin marking of basilic vein’s location by ultrasound. Under local anesthesia, the basilic vein and the cubital vein were dissected free from the arterial anastomosis up to the confluence with the axillary vein, using hook/right-angle retractors to dissect the vein under the skin. The vein was transected peripherally, tunneled subcutaneously in a new lateral route, after a small skin incision in the mid-upper arm, and re-anastomosed. The incisions were closed in a standard fashion. The access is still functional during the last six years. Multiple skip incisions compared to a single long incision have a better cosmetic result and cause less tissue damage. A single incision offers easier vein dissection, needs less operative time but leaves back a longer scar. Multiple skip incisions technique would have the theoretical advantage of reduced postoperative pain, oedema and surgical site infection/dehiscence rates. This is supported in some reports1 but in others, although these complications were encountered infrequently, the difference did not reach statistical significance.
Recurrence of a Resected Carotid Body Tumor Presenting as a Vagal paraganglioma
Purpose: To present a rare case of carotid body tumor recurrence presenting as a vagal paraganglioma. Vagal paragangliomas represent. Case report: An asymptomatic 25-year-old female was diagnosed with a vagal paraganglioma 3 years after an ipsilateral carotid body tumor resection. which had been fully excised as was shown by the pathology specimen examination and a recent Computed Tomography Angiography (CTA). Preoperative presumed diagnosis was based only on duplex scan and CTA. No biopsy was performed because it is contraindicated due to high vascularity of these tumors. Vagal Paraganglioma resection was easily performed because the patient was thin with a clean surgical field locating just distal to the previews operated area. Pathology specimen was conclusive for paraganglioma and his conjunction with the vagus nerve found on operation was indicative for a vagal paraganglioma. The patient remains without recurrence during the last 4 years. Conclusion: This case emphasizes the necessity of a strict postoperative follow-up protocol after resection of paragangliomas, as recurrence is always possible.
Endotension as a Rare Complication to Endovascular Abdominal Aortic Aneurysm Repair.
Papadoulas SI, et al. Innovations (Phila) 2023;18(5):498-502. doi: 10.1177/15569845231191129. Epub 2023 Aug 8. PMID: 37551670. Department of Vascular Surgery, University of Patras Medical School, Patras, Greece
Myasthenia Gravis and Abdominal Aortic Aneurysm: A Rare Combination
Abdominal aortic aneurysm in a patient with myasthenia gravis (MG) is extremely rare. We present a 64-year-old male with MG and an asymptomatic abdominal aortic aneurysm treated endovascularly. After extubation, he suffered a cardiac arrest due to an acute myocardial infarction. Cardiopulmonary resuscitation and a primary coronary angioplasty led to a satisfactory outcome. Special care is needed due to higher rates of postoperative complications in these patients.
Endovascular Repair of an Inflammatory Abdominal Aortic Aneurysm Combined with a Congenital Pelvic Kidney: Case Report and Literature Review.

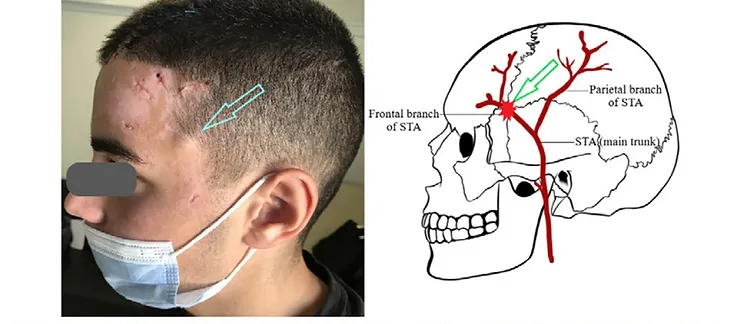
Superficial temporal artery pseudoaneurysm after blunt trauma: A case series
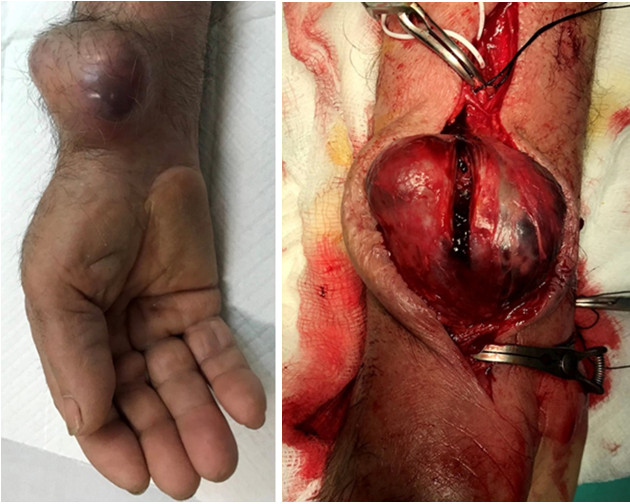
A case report of surgical repair of a post-catheterization radial pseudoaneurysm.
Papadoulas SI, et al. Treatment options for dialysis access steal syndrome.
Patient Transfer with Kocher Forceps on the Axillary Artery: A Rare Case of Ongoing Iatrogenic Vascular Injury.
Treatment of Dialysis Access Steal Syndrome with Concomitant Vascular Access Aneurysms

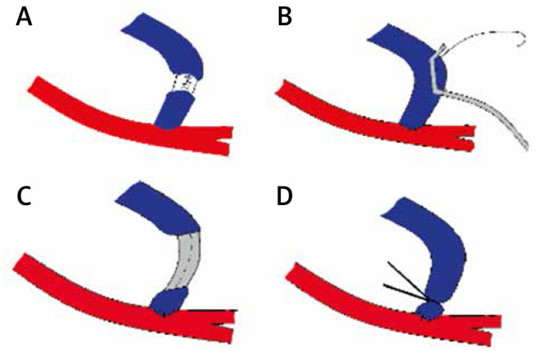
Short interposition grafting for dialysis-access steal syndrome treatment.
Papadoulas S et al. BMJ Case Rep. 2022 Feb 28;15(2):e248446. doi: 10.1136/bcr-2021-248446. Department of Vascular Surgery, University of Patras Medical School, Patras, Greece
Iatrogenic tibial arteriovenous fistula after Fogarty balloon catheter graft thrombectomy
Spyros Papadoulas et al. Clin Case Rep. 2021 Nov 9;9(11):e05050. doi: 10.1002/ccr3.5050. Department of Vascular Surgery, University of Patras Medical School, Patras, Greece

Custom-Made Bifurcated Prosthetic Graft for Aortoiliac Aneurysm Repair
Free-Floating Thrombus in the Distal Internal Carotid Artery Causing a Stroke
Adjunctive vacuum-assisted aspiration thrombectomy in a patient with acute limb ischaemia and peronea arteria magna

A Rare Case of a Small Iliac Aneurysm Causing Iliac Vein Thrombosis
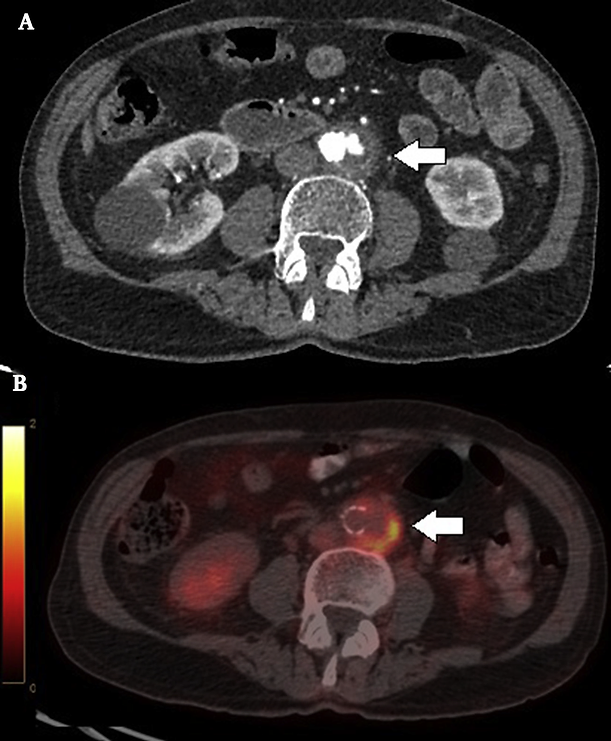
A Mycotic Saccular Aneurysm Diagnosed With 18F-Labelled Fluoro-2-Deoxyglucose Positron Emission Tomography/Computed Tomography Scanning
A Stent Graft Visualised Through an Infected Haemodialysis Graft Pseudoaneurysm
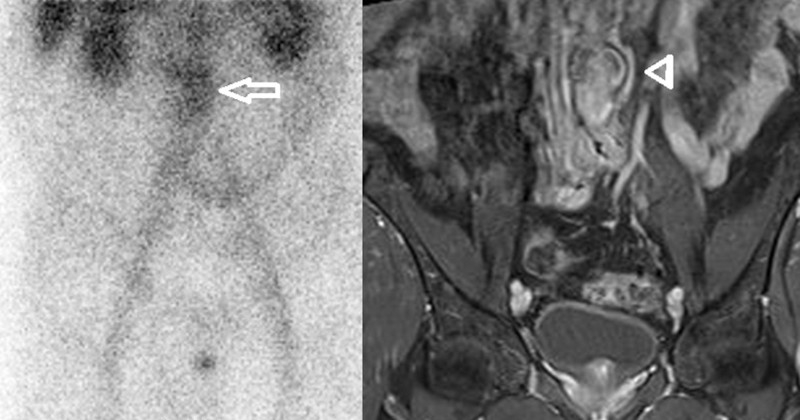
Fever of Unknown Origin due to a Mycotic Abdominal Aortic Aneurysm First Diagnosed with Bone 99mTc Scintigraphy.
Listeriosis infection of an abdominal aortic aneurysm in a diabetic patient.
Retained subintimal pellet in a carotid artery.
Mycotic aneurysm of the internal carotid artery presenting with multiple cerebral septic emboli.
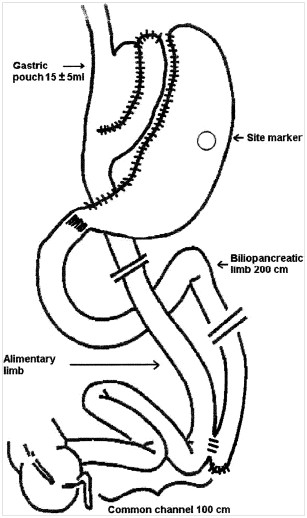
Prospective evaluation of biliopancreatic diversion with Roux-en-Y gastric bypass in the super obese.
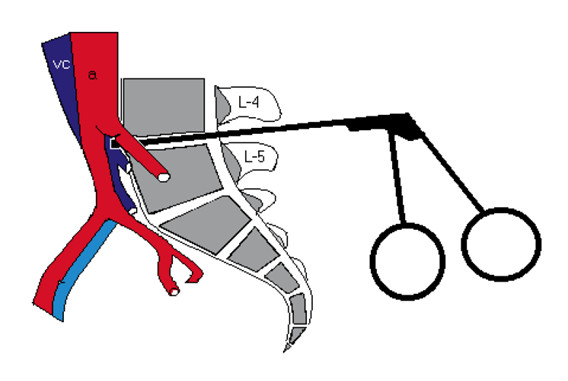
Vascular injury complicating lumbar disc surgery. A systematic review.
Ruptured aneurysms of superficial femoral artery.
Aortocaval fistula in ruptured aneurysms.
Objectives: to study incidence, clinical presentation and problems in management of aortocaval fistula in our series.Design:retrospective study.Materials: during a seven-year period, 112 patients operated on for abdominal aortic aneurysm, including four patients with aortocaval fistula.Methods:standard repair of aortocaval fistula from inside the aneurysmal sac was the preferred operative technique.Results:the incidence of aortocaval fistula was 3.6%. Three cases were found incidentally during emergency surgery for ruptured aneurysms; the fourth case was an isolated aortocaval fistula associated with inferior vena cava thrombosis, diagnosed preoperatively by angiography. In this case, inferior vena cava ligation instead of standard aortocaval repair was performed.Conclusions: Aortocaval fistulas, although rare, should be kept in mind, because clinical diagnosis is often difficult. Furthermore, unsuspected problems during repair may necessitate appropriate change in operative technique.